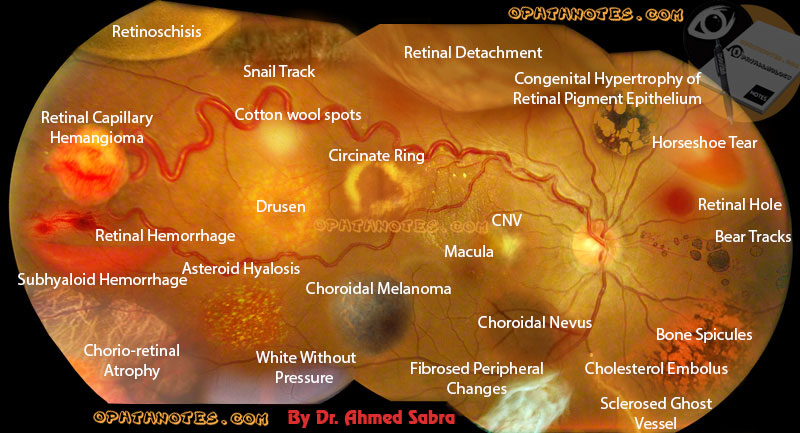
One of the services Optometrics of Chatsworth is proud to offer is that of Digital Retinal Photography. After all, we are strong advocates of preventative health measures, and these high resolution images often help in the diagnoses of ocular diseases that aren't always immediately apparent during the course of a comprehensive eye exam. However, unless you work in the optometry field, they can often be difficult to decipher... until now. Below, some of the signs of retinal disease are shown all in one photo, with an accompanying description. Take a look and see for yourself why retinal photography is such an important service to include during your next eye exam!
Bone spicule pigments (BSP): are a hallmark of retinitis pigmentosa (RP).
Chorioretinal Atrophy: is a condition of the eye where both the choroid and retina are damaged. This causes them to wither away and stop working.
Causes:
Infection is the most common cause of Chorioretinal Atrophy
Inflammation may also damage the Choroid and Retina
Horseshoe tears: Also referred as flap or U-shaped tears are full thickness breaks in the neurosensory retina that occur secondary to vitreous traction.
Bear Tracks: Multiple areas of grouped congenital hypertrophy of the retinal pigment epithelium (CHRPE)
Drusen: (singular, “druse”) are tiny yellow or white accumulations of extracellular material that build up between Bruch’s membraneand the retinal pigment epithelium of the eye. The presence of a few small (“hard”) drusen is normal with advancing age, and most people over 40 have some hard drusen. However, the presence of larger and more numerous drusen in the macula is a common early sign of age-related macular degeneration (AMD).
Choroidal nevi: are benign melanocytic lesions of the posterior uvea. In the United States, their prevalence ranges from 4.6 percent to 7.9 percent in Caucasians. By comparison, choroidal melanoma is rare, manifesting in approximately six in 1 million Caucasian individuals.
Choroidal melanoma: is the most common primary intra-ocular malignant tumor and second most common site of ten malignant melanoma sites in the body.
Exudates: They are the lipid residues of serous leakage from damaged capillaries. The commonest cause is diabetes. Other causes are retinal vein occlusion, angiomas (Von Hippel-Lindau Disease), other vascular dysplasias, and radiation-induced retinal vasculopathy.
Cotton Wool Spots: These yellow-white spots are called cotton wool spots. They are caused by retinal nerve fiber layer microinfarcts. Exploded retinal ganglion cell axons extrude their axoplasm like toothpaste. Expect to find cotton wool spots arrayed around the optic disc and along the temporal vascular arcades. Cotton wool spots have a myriad of causes. Any process that occludes small retinal arterioles will do this: hypertension, diabetes, HIV, severe anemia or thrombocytopenia, hypercoagulable states, connective tissue disorders, viruses, lues, Behçet’s and many others.
Circinate Ring: Exudates very frequently arrange themselves in a circular pattern in diabetes, and often there is a cluster of leaking microaneurysms in the middle of such a ring of exudates.
Vitreous hemorrhage: There are many factors known to cause vitreous hemorrhage.
Diabetic retinopathy The most common cause found in adults is diabetic retinopathy. Abnormal blood vessels can form in the back of the eye of a person with diabetes. These new blood vessels are weaker and prone to breaking and causing hemorrhage.Diabetic retinopathy accounts for 31.5-54% of all cases of vitreous hemorrhage in adults in the United States.
Trauma Some injuries can cause blood vessels in the back of the eye to bleed. Trauma is the leading cause of vitreous hemorrhage in young people, and accounts for 12–18.8% of cases in adults.
Retinal tear or detachment A tear in the retina can allow fluids from the eye to leak in behind the retina, which causes retinal detachment. When this occurs, blood from the retinal blood vessels can bleed into the vitreous. Retinal tear accounts for 11.4–44% of vitreous hemorrhage cases.
Posterior vitreous detachment As one gets older, pockets of fluid can develop in the vitreous. When these pockets develop near the back of the eye, the vitreous can pull away from the retina and possibly tear it.Posterior vitreous detachment accounts for 3.7–11.7% of vitreous hemorrhage cases.
Other causes Less common causes of vitreous hemorrhage make up 6.4–18% of cases, and include:
Asteroid hyalosis: is a degenerative condition of the eye involving small white opacities in the vitreous humor.Clinically, these opacities are quite refractile, giving the appearance of stars (or asteroids) shining in the night sky—except that ocular asteroids are often quite mobile. Ocular asteroids must be distinguished from the more common typical vitreous floaters, which are usually fibrillar or cellular condensates. The cause of asteroid hyalosis is unknown, but it has been associated with diabetes mellitus,hypertension, hypercholesterolemia, The asteroid bodies are made up of hydroxylapatite, which in turn consists ofcalcium and phosphates or phospholipids. While asteroid hyalosis does not usually severely affect vision, the floating opacities can be quite annoying, and may interfere significantly with visualization and testing of the retina. While treatment of asteroid hyalosis is usually unnecessary, vitrectomy may occasionally be indicated, for both diagnostic and therapeutic purposes.
Floaters: are deposits of various size, shape, consistency, refractive index, and motility within the eye’s vitreous humour, which is normally transparent. At a young age, the vitreous is transparent, but as one ages, imperfections gradually develop. The common type of floater, which is present in most person’s eyes, is due to degenerative changes of the vitreous humour. Theperception of floaters is known as myodesopsia,or less commonly as myodaeopsia, myiodeopsia, myiodesopsia. They are also called Muscae volitantes (Latin: “flying flies”), or mouches volantes (from the French). Floaters are visible because of the shadows they cast on the retina or refraction of the light that passes through them, and can appear alone or together with several others in one’s visual field. They may appear as spots, threads, or fragments of cobwebs, which float slowly before the observer’s eyes. As these objects exist within the eye itself, they are not optical illusions but are entoptic phenomena.
Haemangioma: The vascular tumors of the retina and choroid comprise a diverse group of congenital and acquired lesions. The major vascular tumors of the retina include retinal capillary hemangioma, cavernous hemangioma of the retina, retinal vasoproliferative tumor, and racemose hemangiomatosis of the retina or Wyburn–Mason syndrome. Choroidal vascular tumors include circumscribed choroidal hemangioma and diffuse choroidal hemangioma. While classified as benign, visual symptoms secondary to exudative retinal detachment and a variety of other mechanisms are common and are a major source of long-term visual disability. While many therapeutic modalities exist, treatment of symptomatic cases can be challenging. Of particular importance, many of the vascular tumors of the retina and choroid have significant associations with systemic disease. As ocular symptoms are often the most common presenting disease manifestation, the ophthalmologist plays an important role in accurate and early diagnosis. The ability to initiate prompt screening and treatment in appropriate cases is critical. In the following article, the key clinical and diagnostic features of the major retinal and choroidal vascular tumors, their systemic associations, and the literature pertaining to the most currently available treatment strategies are reviewed.
Retinal Hole: Retinal holes and tears are small breaks in the retina. The retina is light-sensitive tissue at the back of the eye. Usually holes and tears do not mean you will have serious vision problems right away. However, retinal holes and tears may cause problems if they allow fluid to seep behind the retina. If a lot of fluid gets behind the retina, the retina can separate from the wall of the eye. The detached part of the retina will not work properly. Detachment of the retina is a serious condition that can lead to total blindness.
Congenital Hypertrophy of RPE (CHRPE): Familial Adenomatous Polyposis (FAP) is an autosomal dominant condition giving rise to multiple adenomatous polyps in the colon which invariably become malignant by the fourth decade. Congenital hypertrophy of retinal pigment epithelium (CHRPE) is one of its extra intestinal manifestations early in childhood seen, present in 90% of FAP population and is easy to detect.
Snail Track: Snail-track retinal degeneration (also known as Schneckenspuren, Milky Way-like, and galaxy-like degeneration) is a vitreoretinal degeneration similar to lattice retinal degeneration. It has the appearance of a white shiny lesion which may be oblong and parallel to the ora serrata or have other shapes and has erosions and holes just like lattice degeneration. The whitish shiny appearance is similar to the slime trail left by a mollusk on the ground and hence its name. It is believed to be akin to lattice degeneration and has the same complications and clinical protocols.
White-Without-Pressure (WSP): WSP is a retinal phenomenon produced by vitreous traction on the surface of the retina . Because it is a superficial phenomenon, it will be more apparent on the green separation. It appears as a whitish degeneration (film) on the retina and typically there is a dark zone along the posterior border (often appears red on binocular indirect ophthalmoscopy which may give the appearance of a pseudo retinal tear). It may have a rather scalloped posterior margin.
Choroidal neovascularization (CNV): is the creation of new blood vessels in the choroid layer of the eye. Choroidal neovascularization is a common cause of neovascular degenerative maculopathy (i.e. ‘wet’ macular degeneration)commonly exacerbated by extreme myopia, malignant myopic degeneration, or age-related developments.
CNV can occur rapidly in individuals with defects in Bruch’s membrane, the innermost layer of the choroid. It is also associated with excessive amounts of Vascular endothelial growth factor (VEGF). As well as in wet macular degeneration, CNV can also occur frequently with the rare genetic disease pseudoxanthoma elasticum and rarely with the more common optic disc drusen. CNV has also been associated with extreme myopia or malignant myopic degeneration, where in choroidal neovascularization occurs primarily in the presence of cracks within the retinal (specifically) macular tissue known as lacquer cracks.
Retinoschisis: Retinoschisis is an eye disease characterized by the abnormal splitting of the retina’s neurosensory layers, usually in the outer plexiform layer. Most common forms are asymptomatic, some rarer forms result in a loss of vision in the corresponding visual field.
Classification
This article originally appeared on opthnotes.com
Chorioretinal Atrophy: is a condition of the eye where both the choroid and retina are damaged. This causes them to wither away and stop working.
Causes:
Infection is the most common cause of Chorioretinal Atrophy
- Toxoplasmosis
- Toxocara
- Cytomegalovirus
- Cold Sore Virus
- Chicken Pox Virus
Inflammation may also damage the Choroid and Retina
Horseshoe tears: Also referred as flap or U-shaped tears are full thickness breaks in the neurosensory retina that occur secondary to vitreous traction.
Bear Tracks: Multiple areas of grouped congenital hypertrophy of the retinal pigment epithelium (CHRPE)
Drusen: (singular, “druse”) are tiny yellow or white accumulations of extracellular material that build up between Bruch’s membraneand the retinal pigment epithelium of the eye. The presence of a few small (“hard”) drusen is normal with advancing age, and most people over 40 have some hard drusen. However, the presence of larger and more numerous drusen in the macula is a common early sign of age-related macular degeneration (AMD).
Choroidal nevi: are benign melanocytic lesions of the posterior uvea. In the United States, their prevalence ranges from 4.6 percent to 7.9 percent in Caucasians. By comparison, choroidal melanoma is rare, manifesting in approximately six in 1 million Caucasian individuals.
Choroidal melanoma: is the most common primary intra-ocular malignant tumor and second most common site of ten malignant melanoma sites in the body.
Exudates: They are the lipid residues of serous leakage from damaged capillaries. The commonest cause is diabetes. Other causes are retinal vein occlusion, angiomas (Von Hippel-Lindau Disease), other vascular dysplasias, and radiation-induced retinal vasculopathy.
Cotton Wool Spots: These yellow-white spots are called cotton wool spots. They are caused by retinal nerve fiber layer microinfarcts. Exploded retinal ganglion cell axons extrude their axoplasm like toothpaste. Expect to find cotton wool spots arrayed around the optic disc and along the temporal vascular arcades. Cotton wool spots have a myriad of causes. Any process that occludes small retinal arterioles will do this: hypertension, diabetes, HIV, severe anemia or thrombocytopenia, hypercoagulable states, connective tissue disorders, viruses, lues, Behçet’s and many others.
Circinate Ring: Exudates very frequently arrange themselves in a circular pattern in diabetes, and often there is a cluster of leaking microaneurysms in the middle of such a ring of exudates.
Vitreous hemorrhage: There are many factors known to cause vitreous hemorrhage.
Diabetic retinopathy The most common cause found in adults is diabetic retinopathy. Abnormal blood vessels can form in the back of the eye of a person with diabetes. These new blood vessels are weaker and prone to breaking and causing hemorrhage.Diabetic retinopathy accounts for 31.5-54% of all cases of vitreous hemorrhage in adults in the United States.
Trauma Some injuries can cause blood vessels in the back of the eye to bleed. Trauma is the leading cause of vitreous hemorrhage in young people, and accounts for 12–18.8% of cases in adults.
Retinal tear or detachment A tear in the retina can allow fluids from the eye to leak in behind the retina, which causes retinal detachment. When this occurs, blood from the retinal blood vessels can bleed into the vitreous. Retinal tear accounts for 11.4–44% of vitreous hemorrhage cases.
Posterior vitreous detachment As one gets older, pockets of fluid can develop in the vitreous. When these pockets develop near the back of the eye, the vitreous can pull away from the retina and possibly tear it.Posterior vitreous detachment accounts for 3.7–11.7% of vitreous hemorrhage cases.
Other causes Less common causes of vitreous hemorrhage make up 6.4–18% of cases, and include:
- Proliferative sickle cell retinopathy
- Macroaneurysm
- Age-related macular degeneration
- Terson syndrome
- Retinal neovascularization as a result of branch or central retinal vein occlusion
- Other – about 7 cases in 100,000 have no known cause attributed to them.
Asteroid hyalosis: is a degenerative condition of the eye involving small white opacities in the vitreous humor.Clinically, these opacities are quite refractile, giving the appearance of stars (or asteroids) shining in the night sky—except that ocular asteroids are often quite mobile. Ocular asteroids must be distinguished from the more common typical vitreous floaters, which are usually fibrillar or cellular condensates. The cause of asteroid hyalosis is unknown, but it has been associated with diabetes mellitus,hypertension, hypercholesterolemia, The asteroid bodies are made up of hydroxylapatite, which in turn consists ofcalcium and phosphates or phospholipids. While asteroid hyalosis does not usually severely affect vision, the floating opacities can be quite annoying, and may interfere significantly with visualization and testing of the retina. While treatment of asteroid hyalosis is usually unnecessary, vitrectomy may occasionally be indicated, for both diagnostic and therapeutic purposes.
Floaters: are deposits of various size, shape, consistency, refractive index, and motility within the eye’s vitreous humour, which is normally transparent. At a young age, the vitreous is transparent, but as one ages, imperfections gradually develop. The common type of floater, which is present in most person’s eyes, is due to degenerative changes of the vitreous humour. Theperception of floaters is known as myodesopsia,or less commonly as myodaeopsia, myiodeopsia, myiodesopsia. They are also called Muscae volitantes (Latin: “flying flies”), or mouches volantes (from the French). Floaters are visible because of the shadows they cast on the retina or refraction of the light that passes through them, and can appear alone or together with several others in one’s visual field. They may appear as spots, threads, or fragments of cobwebs, which float slowly before the observer’s eyes. As these objects exist within the eye itself, they are not optical illusions but are entoptic phenomena.
Haemangioma: The vascular tumors of the retina and choroid comprise a diverse group of congenital and acquired lesions. The major vascular tumors of the retina include retinal capillary hemangioma, cavernous hemangioma of the retina, retinal vasoproliferative tumor, and racemose hemangiomatosis of the retina or Wyburn–Mason syndrome. Choroidal vascular tumors include circumscribed choroidal hemangioma and diffuse choroidal hemangioma. While classified as benign, visual symptoms secondary to exudative retinal detachment and a variety of other mechanisms are common and are a major source of long-term visual disability. While many therapeutic modalities exist, treatment of symptomatic cases can be challenging. Of particular importance, many of the vascular tumors of the retina and choroid have significant associations with systemic disease. As ocular symptoms are often the most common presenting disease manifestation, the ophthalmologist plays an important role in accurate and early diagnosis. The ability to initiate prompt screening and treatment in appropriate cases is critical. In the following article, the key clinical and diagnostic features of the major retinal and choroidal vascular tumors, their systemic associations, and the literature pertaining to the most currently available treatment strategies are reviewed.
Retinal Hole: Retinal holes and tears are small breaks in the retina. The retina is light-sensitive tissue at the back of the eye. Usually holes and tears do not mean you will have serious vision problems right away. However, retinal holes and tears may cause problems if they allow fluid to seep behind the retina. If a lot of fluid gets behind the retina, the retina can separate from the wall of the eye. The detached part of the retina will not work properly. Detachment of the retina is a serious condition that can lead to total blindness.
Congenital Hypertrophy of RPE (CHRPE): Familial Adenomatous Polyposis (FAP) is an autosomal dominant condition giving rise to multiple adenomatous polyps in the colon which invariably become malignant by the fourth decade. Congenital hypertrophy of retinal pigment epithelium (CHRPE) is one of its extra intestinal manifestations early in childhood seen, present in 90% of FAP population and is easy to detect.
Snail Track: Snail-track retinal degeneration (also known as Schneckenspuren, Milky Way-like, and galaxy-like degeneration) is a vitreoretinal degeneration similar to lattice retinal degeneration. It has the appearance of a white shiny lesion which may be oblong and parallel to the ora serrata or have other shapes and has erosions and holes just like lattice degeneration. The whitish shiny appearance is similar to the slime trail left by a mollusk on the ground and hence its name. It is believed to be akin to lattice degeneration and has the same complications and clinical protocols.
White-Without-Pressure (WSP): WSP is a retinal phenomenon produced by vitreous traction on the surface of the retina . Because it is a superficial phenomenon, it will be more apparent on the green separation. It appears as a whitish degeneration (film) on the retina and typically there is a dark zone along the posterior border (often appears red on binocular indirect ophthalmoscopy which may give the appearance of a pseudo retinal tear). It may have a rather scalloped posterior margin.
Choroidal neovascularization (CNV): is the creation of new blood vessels in the choroid layer of the eye. Choroidal neovascularization is a common cause of neovascular degenerative maculopathy (i.e. ‘wet’ macular degeneration)commonly exacerbated by extreme myopia, malignant myopic degeneration, or age-related developments.
CNV can occur rapidly in individuals with defects in Bruch’s membrane, the innermost layer of the choroid. It is also associated with excessive amounts of Vascular endothelial growth factor (VEGF). As well as in wet macular degeneration, CNV can also occur frequently with the rare genetic disease pseudoxanthoma elasticum and rarely with the more common optic disc drusen. CNV has also been associated with extreme myopia or malignant myopic degeneration, where in choroidal neovascularization occurs primarily in the presence of cracks within the retinal (specifically) macular tissue known as lacquer cracks.
Retinoschisis: Retinoschisis is an eye disease characterized by the abnormal splitting of the retina’s neurosensory layers, usually in the outer plexiform layer. Most common forms are asymptomatic, some rarer forms result in a loss of vision in the corresponding visual field.
Classification
- Hereditary
- X linked juvenile retinoschisis
- Familial foveal retinoschisis
- Tractional
- Exudative
- Secondary to Optic disc pit
- Degenerative
- Typical
- Reticular
This article originally appeared on opthnotes.com